- Home
- About Us
- Services
- Treatments
- Acid Reflux
- Allergic Rhinitis
- Alcoholic Fatty Liver
- Ankylosing Spondylitis
- Anxiety / Stress
- Arthritis
- Asthma
- Cervical Spondylitis
- Celiac Infection
- Colitis
- Constipation
- Dermatitis
- Detox Programme
- Diabetes (Madhumeha)
- Hair Fall
- Headache
- Hormonal Imbalance
- Hypertension
- Insomnia
- Irritable Bowel Syndrome
- Lungs Disease
- Migraine
- Neurological Disorder
- Non Alcoholic Fatty Liver
- Obesity Management
- Pain Management
- PCOD
- PCOS
- Sciatica Pain
- Sinusitis
- Skin Disorder
- Slip Disc
- Stress Management
- Thyroid
- Weight Management
- Techno-Ayurveda
- Media
- Blog
- Contact Us
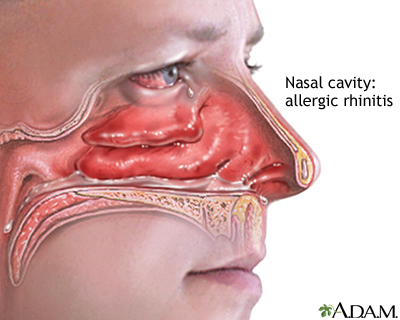
Allergic Rhinitis
Understanding Allergic Rhinitis
In Ayurveda, allergic rhinitis is seen as an imbalance between the doshas, particularly Kapha and Vata. Kapha is associated with the production of mucus, and when it becomes aggravated, it can lead to excessive mucus secretion, causing congestion and nasal discharge. Vata dosha governs the air and movement in the body, and when it is out of balance, it can lead to dryness in the nasal passages, further aggravating symptoms like sneezing and itching.
From an Ayurvedic perspective, allergic rhinitis is often a result of accumulated toxins (or ama) in the body, weak digestion (Mandagni), and a compromised immune system. These toxins may be triggered by environmental allergens, dietary factors, or stress, leading to inflammation and hypersensitivity reactions in the nasal passages.
Types of Allergic Rhinitis
Seasonal Allergic Rhinitis
Seasonal allergic rhinitis, commonly referred to as hay fever, is a type of allergic rhinitis that occurs during specific seasons of the year when certain allergens, particularly pollen, are in the air. It is caused by an allergic reaction to airborne substances like pollen from trees, grasses, or weeds. This type of rhinitis is one of the most common forms of allergies and typically causes symptoms such as sneezing, nasal congestion, a runny nose, itchy eyes, and post-nasal drip.
Perennial Allergic Rhinitis
Perennial allergic rhinitis is a type of allergic rhinitis that occurs year-round, as opposed to seasonal allergic rhinitis, which only occurs during specific times of the year. This chronic condition is caused by the body's immune system reacting to allergens that are present in the environment throughout the year, such as dust mites, pet dander, mold, or cockroach droppings. People with perennial allergic rhinitis often experience persistent symptoms that can affect their quality of life and may require ongoing management.
Exposure to Irritants
Sinus-related allergic rhinitis refers to a condition where allergic rhinitis (inflammation of the nasal passages due to allergens) leads to inflammation of the sinuses, resulting in sinus-related symptoms. This condition is often referred to as allergic rhinosinusitis, and it occurs when airborne allergens, such as pollen, dust mites, mold, or pet dander, trigger inflammation not just in the nasal passages but also in the sinus cavities.
Cold-Related Allergic Rhinitis
Cold-related allergic rhinitis refers to the exacerbation of allergy symptoms that can occur during cold weather or when exposed to cold air. This condition is sometimes called non-seasonal allergic rhinitis or vasomotor rhinitis, and it occurs when allergens and environmental changes, such as cold air or dry indoor heating, trigger the immune system, causing inflammation in the nasal passages. While not caused by cold viruses, it can feel similar to a cold, with symptoms like a runny nose, sneezing, nasal congestion, and itching.
Food-Induced Allergic Rhinitis
Food-induced allergic rhinitis refers to an allergic reaction that affects the nasal passages as a result of consuming certain foods. While food allergies are more commonly associated with severe symptoms like anaphylaxis, some individuals may experience milder allergic reactions that primarily affect the nasal passages, leading to symptoms similar to those of typical allergic rhinitis. These symptoms can include sneezing, a runny nose, nasal congestion, and itchy eyes or throat.
Symptoms of Allergic Rhinitis
1. Sneezing
2. Itchy or Watery Eyes
3. Nasal Congestion
4. Runny Nose
5. Postnasal Drip
6. Itchy Throat or Ears
Common Causes of Allergic Rhinitis

Environmental Allergens
Environmental allergens like pollen, mold, pet dander, and dust mites trigger allergic rhinitis by causing an immune response. These allergens irritate the nasal passages, leading to inflammation, congestion, sneezing, and a runny nose, common symptoms of the condition.

Weather Changes
Weather changes can trigger allergic rhinitis by increasing exposure to allergens like pollen, mold, and dust. Sudden shifts in temperature or humidity affect airborne particles, leading to inflammation in the nasal passages, causing symptoms like sneezing, congestion, and itching.

Exposure to Irritants
Exposure to irritants like smoke, strong odors, pollution, and chemicals can trigger allergic rhinitis. These irritants inflame the nasal passages, leading to symptoms such as sneezing, congestion, runny nose, and itchy eyes, worsening allergy reactions.

Dietary Factors
Dietary factors can contribute to allergic rhinitis by triggering immune responses. Certain foods, like those high in histamines or allergens such as dairy, eggs, or nuts, may exacerbate symptoms. Inflammatory foods can also worsen overall immune system function.

Lifestyle Factors
Lifestyle factors such as exposure to allergens in the home (dust mites, pet dander), smoking, poor indoor air quality, and lack of regular cleaning can trigger or worsen allergic rhinitis. Stress, inadequate sleep, and a poor diet may also contribute.

Genetics and Family History
Genetics play a significant role in allergic rhinitis, with family history influencing susceptibility. Individuals with parents or siblings who have allergies are more likely to develop the condition. Inherited immune system sensitivities contribute to the body's allergic reactions.

Immune System Weakness
Immune system weakness can contribute to allergic rhinitis by impairing the body's ability to regulate allergic reactions. When the immune system is compromised, it may overreact to environmental allergens, triggering inflammation and symptoms like sneezing, congestion, and itching.
FAQs of Allergic Rhinitis
Allergic rhinitis is an inflammation of the nasal passages triggered by allergens such as pollen, dust, mold, or pet dander.
Symptoms include sneezing, nasal congestion, runny nose, itchy or watery eyes, and post-nasal drip.
Treatment includes antihistamines, nasal decongestants, corticosteroid nasal sprays, allergy shots (immunotherapy), and avoiding allergens.
